What Is Microdosing MDMA and Is It Dangerous?
Aliya
on
October 11, 2023
In recent years, microdosing has gained popularity as an alternative way to experience the effects of many substances, including MDMA, a drug commonly known as ecstasy. If you are wondering, “What does it mean to dose MDMA,” it’s important to know what microdosing MDMA entails, as well as the effects of MDMA on the body.
What Is MDMA?
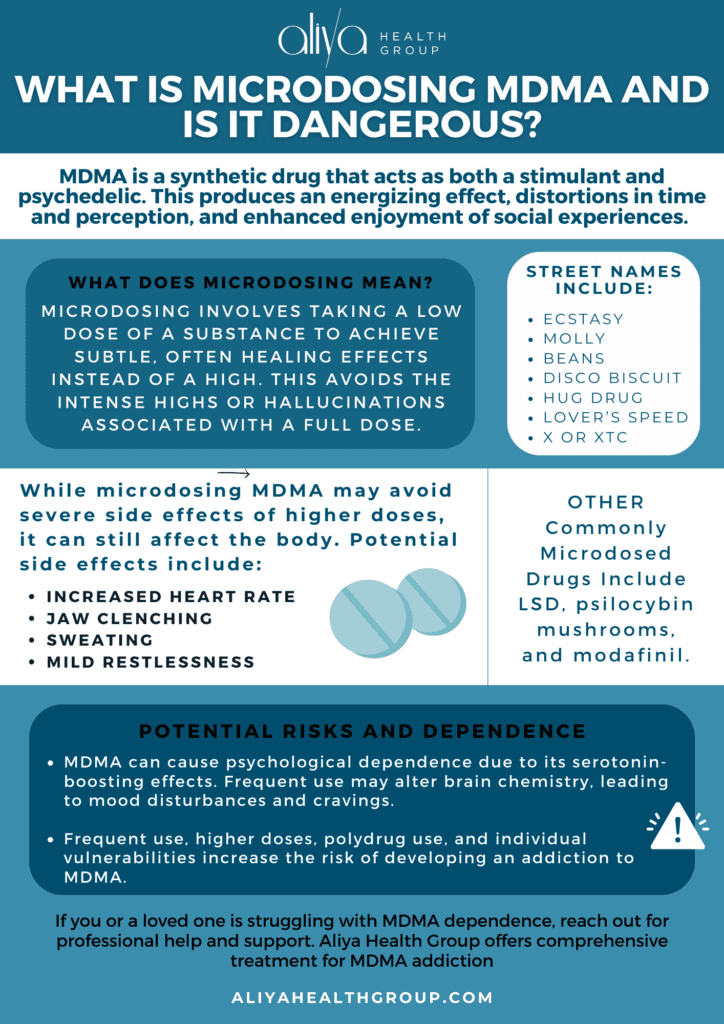
According to the National Institute on Drug Abuse, MDMA, short for 3,4-methylenedioxymethamphetamine, is a synthetic drug that acts as both a stimulant and psychedelic. This produces an energizing effect, distortions in time and perception, and enhanced enjoyment of social experiences. The drug was originally developed to help control bleeding, but over time, it gained popularity in the recreational drug scene due to its pleasurable effects. People who use MDMA often do so in social or party settings, as it can enhance feelings of connection and sociability.
As of 2021, around 21.1 million people in the United States had used MDMA at some point in their lifetime. While commonly referred to as “ecstasy” or “Molly,” other slang terms include Adam, Beans, Clarity, Disco Biscuit, E, Eve, Go, Hug Drug, Lover’s Speed, Peace, STP, X, and XTC.
What Does Microdosing Mean?
Microdosing involves taking a low dose of a substance to achieve subtle, often healing effects instead of a high. This avoids the intense highs or hallucinations associated with a full dose. There isn’t a single, clearly recognized definition of microdosing for any drug, but one definition states it’s approximately 1/5 to 1/20 of a recreational dose.
Microdosing vs. Full Dosing
When someone microdoses MDMA, they aim to experience the potential medicinal benefits of the drug without the overwhelming effects of a standard recreational dose. A full dose of MDMA can cause intense euphoria, heightened senses, and emotional openness. Microdosing, on the other hand, is intended to be “subperceptual,” meaning the effects are not consciously felt.
Commonly Microdosed Drugs
In addition to MDMA, other substances that are commonly microdosed include psychedelics like LSD and psilocybin mushrooms, as well as stimulants like modafinil.
What Happens When You Microdose MDMA?
The effects of microdosing MDMA can lead to subtle feelings that are not overwhelming. Some people report increased sociability, improved mood, heightened sensory perception, and enhanced empathy. However, these effects are generally less notable than those experienced with a full dose of MDMA. Some use microdosing to help with stress disorders. Post-traumatic stress disorder is one such stress disorder (PTSD). Experimental treatment using MDMA-assisted psychotherapy is a new form of treatment that doesn’t have much research surrounding its effectiveness.
Side Effects of Microdosing MDMA
While microdosing MDMA may not lead to the severe side effects associated with higher doses, it can still negatively affect the body.
Potential side effects of microdosing MDMA include:
- Increased heart rate
- Jaw clenching
- Sweating
- Mild restlessness
These side effects are usually less intense than what one might experience with recreational use.
What Factors Impact the Effects of MDMA?
As with all illicit street drugs, the strength and duration of MDMA can vary from one MDMA dose to the next. Without safety regulations and quality control, people who buy MDMA (and even those who sell it) don’t always know exactly what they’re getting. This makes it difficult to predict how a person will react to the drug, especially when microdosing.
Additionally, there are several factors that can influence the effects of MDMA, including:
- Body weight and composition
- Metabolism
- Genetics
- Tolerance
- Environmental factors (such as temperature and noise)
It’s important to keep in mind that even with proper research and precautions, there is still a risk of adverse reactions or negative side effects when using MDMA for any purpose.
With that said, some individuals may notice some improvements in mood and focus shortly after microdosing. Others may not perceive any noticeable effects of MDMA when microdosing. In general, the duration of microdosing effects is shorter than a full MDMA experience, often lasting a few hours.
Get confidential help from our addiction and mental health treatment facilities located across the United States. Call to join one of our quality programs today!
Speak With Our Admissions TeamIs MDMA Addictive?
MDMA has the potential for psychological dependence, although it is considered to be less addictive than some other drugs, such as opioids or stimulants like cocaine. The addictive nature of MDMA is mainly caused by its pleasurable effect on mood and emotions, which happens when the brain increases the release of neurotransmitters like serotonin (also known as as the “happy” chemical).
Over time, frequent MDMA abuse can lead to changes in the brain’s chemistry, potentially resulting in negative mood disturbances and cravings.
Risk Factors for Addiction
Several factors can increase the risk of developing an addiction to MDMA:
- Frequency of use: The more frequently MDMA is used, the greater the risk of developing tolerance and dependence.
- Dosage: Higher doses of MDMA can lead to more intense effects and may increase the risk of addiction.
- Polydrug Use: Using MDMA in combination with other substances, such as alcohol or other drugs, can speed up the risk of addiction and other health complications.
- Individual vulnerability: Some people may be more susceptible to addiction due to genetic, environmental, or psychological factors.
MDMA Addiction Treatment
If you or a loved one has developed an addiction from microdosing MDMA, Aliya Health Group, one of the leading treatment centers for mental health and addiction, is here to help. We’re dedicated to providing comprehensive treatment options for individuals struggling with MDMA addiction and related issues.
Our experienced addiction treatment professionals conduct thorough assessments to understand your unique needs and challenges. These assessments assist in the development of your personalized addiction and mental health treatment plan.
Our MDMA treatment approach includes:
- Detox
- Residential mental health treatment
- Outpatient treatment
- Aftercare programs and support services
Many individuals with MDMA addiction also struggle with co-occurring mental health issues. To help clients fully recover, dual diagnosis treatment can provide addiction recovery services and inpatient mental health treatment to both address co-occurring disorders.
Drug Detox
If you’re psychologically or physically dependent on MDMA, a medical detox program can help you recover. A medically supervised detox process ensures the safe and comfortable elimination of the drug from the body. These drug detox programs can offer a range of supportive services to help ease withdrawal symptoms and provide emotional support during this challenging time.
Residential Treatment
The most intensive form of addiction treatment involves living full-time at an inpatient drug rehab center. Residential treatment assists with both drugs and alcohol and behavioral health. It involves psychotherapy in individual and group settings. Behavioral therapy, including individual and group counseling, is a cornerstone of our holistic mental health treatment approach. Therapy can help address the psychological aspects of addiction, develop coping strategies, and foster a support network.
Outpatient Treatment
After inpatient rehab, many MDMA addiction treatment centers offer outpatient treatment to significantly reduce the risk of relapse. Outpatient rehab involves many of the treatments and therapies offered in inpatient care, as well as teaching life skills and coping mechanisms to avoid drugs and alcohol in the future.
Aftercare and Relapse Prevention
The journey to recovery doesn’t end after completing treatment. For this reason, aftercare programs offer ongoing support, counseling, and resources to help you maintain sobriety and build a fulfilling life.
Schedule a Consultation
Some may find benefits in the effects of Microdosing MDMA, but it doesn’t come without risks. Even a low dose can lead to something more concerning. If you or someone you know is struggling with a dependence on MDMA, don’t hesitate to reach out to one of our addiction treatment and mental health treatment facilities for help. You’re not alone, and there are resources available to guide you on the path to recovery. Contact us today to verify your insurance and put a stop to drug abuse once and for all.
- MDMA (Ecstasy/Molly) DrugFacts | National Institute on Drug Abuse (NIDA) (nih.gov)
- What is the history of MDMA? | National Institute on Drug Abuse (NIDA) (nih.gov)
- Lifetime ecstasy users U.S. 2009-2021 | Statista
- Drug Fact Sheet: Ectasty/MDMA (dea.gov)
- Microdosing psychedelics: More questions than answers? An overview and suggestions for future research – Kim PC Kuypers, Livia Ng, David Erritzoe, Gitte M Knudsen, Charles D Nichols, David E Nichols, Luca Pani, Anaïs Soula, David Nutt, 2019 (sagepub.com)
- Paradoxical effects of low dose MDMA on latent inhibition in the rat – PMC (nih.gov)